
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Hypoxia Increases β-Cell Death by Activating Pancreatic Stellate Cells within the Islet
- Jong Jin Kim, Esder Lee, Gyeong Ryul Ryu, Seung-Hyun Ko, Yu-Bae Ahn, Ki-Ho Song
- Diabetes Metab J. 2020;44(6):919-927. Published online May 11, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0181
- 5,970 View
- 146 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
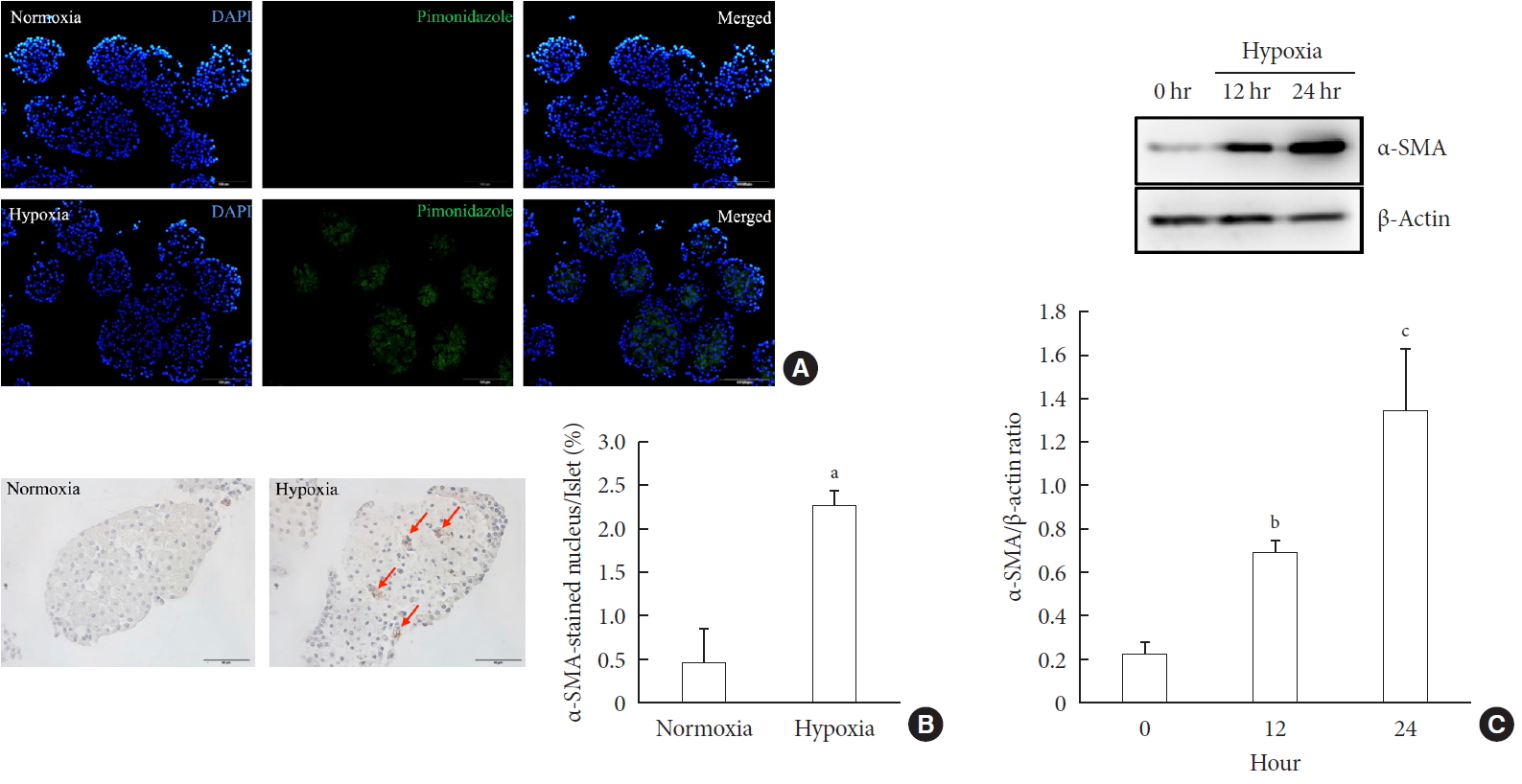
ePub Background Hypoxia can occur in pancreatic islets in type 2 diabetes mellitus. Pancreatic stellate cells (PSCs) are activated during hypoxia. Here we aimed to investigate whether PSCs within the islet are also activated in hypoxia, causing β-cell injury.
Methods Islet and primary PSCs were isolated from Sprague Dawley rats, and cultured in normoxia (21% O2) or hypoxia (1% O2). The expression of α-smooth muscle actin (α-SMA), as measured by immunostaining and Western blotting, was used as a marker of PSC activation. Conditioned media (hypoxia-CM) were obtained from PSCs cultured in hypoxia.
Results Islets and PSCs cultured in hypoxia exhibited higher expressions of α-SMA than did those cultured in normoxia. Hypoxia increased the production of reactive oxygen species. The addition of N-acetyl-L-cysteine, an antioxidant, attenuated the hypoxia-induced PSC activation in islets and PSCs. Islets cultured in hypoxia-CM showed a decrease in cell viability and an increase in apoptosis.
Conclusion PSCs within the islet are activated in hypoxia through oxidative stress and promote islet cell death, suggesting that hypoxia-induced PSC activation may contribute to β-cell loss in type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Effects of hypoxia in the diabetic corneal stroma microenvironment
Purnima Sharma, Jian-Xing Ma, Dimitrios Karamichos
Experimental Eye Research.2024; 240: 109790. CrossRef - Visualizing hypoxic modulation of beta cell secretions via a sensor augmented oxygen gradient
Kai Duan, Mengyang Zhou, Yong Wang, Jose Oberholzer, Joe F. Lo
Microsystems & Nanoengineering.2023;[Epub] CrossRef - Pancreatic stellate cells promote pancreatic β-cell death through exosomal microRNA transfer in hypoxia
Esder Lee, Gyeong Ryul Ryu, Seung-Hyun Ko, Yu-Bae Ahn, Ki-Ho Song
Molecular and Cellular Endocrinology.2023; 572: 111947. CrossRef - Pancreatic stellate cells in pancreatic cancer: as potential targets for future therapy
Zhengfeng Wang, Ru He, Shi Dong, Wence Zhou
Frontiers in Oncology.2023;[Epub] CrossRef - Recent advances in the development of bioartificial pancreas using 3D bioprinting for the treatment of type 1 diabetes: a review
Anushikha Ghosh, Arka Sanyal, Abhik Mallick
Exploration of Medicine.2023; : 886. CrossRef - Pancreas and islet morphology in cystic fibrosis: clues to the etiology of cystic fibrosis-related diabetes
Sarah S. Malik, Diksha Padmanabhan, Rebecca L. Hull-Meichle
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diabetic mellitus, vascular calcification and hypoxia: A complex and neglected tripartite relationship
Xue-Jiao Sun, Nai-Feng Liu
Cellular Signalling.2022; 91: 110219. CrossRef - HIF-1 and NRF2; Key Molecules for Malignant Phenotypes of Pancreatic Cancer
Shin Hamada, Ryotaro Matsumoto, Atsushi Masamune
Cancers.2022; 14(2): 411. CrossRef - Pancreatic Stellate Cells and Metabolic Alteration: Physiology and Pathophysiology
Shin Hamada, Ryotaro Matsumoto, Atsushi Masamune
Frontiers in Physiology.2022;[Epub] CrossRef - Exosomal miR-140–3p and miR-143–3p from TGF-β1-treated pancreatic stellate cells target BCL2 mRNA to increase β-cell apoptosis
Xiangyun Zhu, Dechen Liu, Guoqing Li, Mengmeng Zhi, Ji Sun, Liang Qi, Jingbo Li, Stephen J. Pandol, Ling Li
Molecular and Cellular Endocrinology.2022; 551: 111653. CrossRef - Mitochondria oxidative stress mediated nicotine-promoted activation of pancreatic stellate cells by regulating mitochondrial dynamics
Yue Yuan, Zhiren Li, Miaomiao Li, Tong Jin, Xiaoyun Zhang, Xinjuan Liu, Jianyu Hao
Toxicology in Vitro.2022; 84: 105436. CrossRef - Antioxidant Mitoquinone Alleviates Chronic Pancreatitis via Anti-Fibrotic and Antioxidant Effects
Miaomiao Li, Yue Yuan, Xue Han, Xinjuan Liu, Weizhen Zhang, Jianyu Hao
Journal of Inflammation Research.2022; Volume 15: 4409. CrossRef - Diabetic Ferroptosis and Pancreatic Cancer: Foe or Friend?
Le Li, Xing-jia Yu, Lei Gao, Long Cheng, Bei Sun, Gang Wang
Antioxidants & Redox Signaling.2022; 37(16-18): 1206. CrossRef - Melatonin Induces Apoptosis and Modulates Cyclin Expression and MAPK Phosphorylation in Pancreatic Stellate Cells Subjected to Hypoxia
Matias Estaras, Manuel R. Gonzalez-Portillo, Miguel Fernandez-Bermejo, Jose M. Mateos, Daniel Vara, Gerardo Blanco-Fernandez, Diego Lopez-Guerra, Vicente Roncero, Gines M. Salido, Antonio González
International Journal of Molecular Sciences.2021; 22(11): 5555. CrossRef - Integrated pancreatic microcirculatory profiles of streptozotocin‐induced and insulin‐administrated type 1 diabetes mellitus
Yuan Li, Bingwei Li, Bing Wang, Mingming Liu, Xiaoyan Zhang, Ailing Li, Jian Zhang, Honggang Zhang, Ruijuan Xiu
Microcirculation.2021;[Epub] CrossRef - Pancreatic stellate cells - rising stars in pancreatic pathologies
P Hrabák, M Kalousová, T Krechler, T Zima
Physiological Research.2021; (S4): S597. CrossRef
- Effects of hypoxia in the diabetic corneal stroma microenvironment
- Protective Effect of Heme Oxygenase-1 on High Glucose-Induced Pancreatic β-Cell Injury
- Eun-Mi Lee, Young-Eun Lee, Esder Lee, Gyeong Ryul Ryu, Seung-Hyun Ko, Sung-Dae Moon, Ki-Ho Song, Yu-Bae Ahn
- Diabetes Metab J. 2011;35(5):469-479. Published online October 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.5.469
- 3,700 View
- 35 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Glucose toxicity that is caused by chronic exposure to a high glucose concentration leads to islet dysfunction and induces apoptosis in pancreatic β-cells. Heme oxygenase-1 (HO-1) has been identified as an anti-apoptotic and cytoprotective gene. The purpose of this study is to investigate whether HO-1 up-regulation when using metalloprotophyrin (cobalt protoporphyrin, CoPP) could protect pancreatic β-cells from high glucose-induced apoptosis.
Methods Reverse transcription-polymerase chain reaction was performed to analyze the CoPP-induced mRNA expression of HO-1. Cell viability of INS-1 cells cultured in the presence of CoPP was examined by acridine orange/propidium iodide staining. The generation of intracellular reactive oxygen species (ROS) was measured using flow cytometry. Glucose stimulated insulin secretion (GSIS) was determined following incubation with CoPP in different glucose concentrations.
Results CoPP increased HO-1 mRNA expression in both a dose- and time-dependent manner. Overexpression of HO-1 inhibited caspase-3, and the number of dead cells in the presence of CoPP was significantly decreased when exposed to high glucose conditions (HG). CoPP also decreased the generation of intracellular ROS by 50% during 72 hours of culture with HG. However, decreased GSIS was not recovered even in the presence of CoPP.
Conclusion Our data suggest that CoPP-induced HO-1 up-regulation results in protection from high glucose-induced apoptosis in INS-1 cells; however, glucose stimulated insulin secretion is not restored.
-
Citations
Citations to this article as recorded by- Diabetes: Risk factor and translational therapeutic implications for Alzheimer's disease
Jeffrey Cummings, Andrew Ortiz, Janelle Castellino, Jefferson Kinney
European Journal of Neuroscience.2022; 56(9): 5727. CrossRef - The ischaemic preconditioning paradox and its implications for islet isolation from heart-beating and non heart-beating donors
Daniel Brandhorst, Heide Brandhorst, Samuel Acreman, Paul R. V. Johnson
Scientific Reports.2022;[Epub] CrossRef - CYTOCHROMES OF MITOCHONDRIES AND ACTIVITY OF HEME METABOLISM ENZYMES IN THE LIVER UNDER DIFFERENT NUTRIENT REGIMES
G.P. Kopylchuk, Z.-M. I. Grynenkiv, O.M. Voloshchuk
Fiziolohichnyĭ zhurnal.2021; 67(2): 37. CrossRef - Heme Oxygenase-1 (HMOX-1) and inhibitor of differentiation proteins (ID1, ID3) are key response mechanisms against iron-overload in pancreatic β-cells
Mawieh Hamad, Abdul Khader Mohammed, Mahmood Y. Hachim, Debasmita Mukhopadhy, Anila Khalique, Amina Laham, Sarah Dhaiban, Khuloud Bajbouj, Jalal Taneera
Molecular and Cellular Endocrinology.2021; 538: 111462. CrossRef - Food-derived cyanidin-3-O-glucoside alleviates oxidative stress: evidence from the islet cell line and diabetic db/db mice
Xiang Ye, Wen Chen, Pengcheng Tu, Ruoyi Jia, Yangyang Liu, Yonglu Li, Qiong Tang, Xiaodong Zheng, Qiang Chu
Food & Function.2021; 12(22): 11599. CrossRef - Telmisartan protects against high glucose/high lipid‐induced apoptosis and insulin secretion by reducing the oxidative and ER stress
Yan Wang, Jingjing Xue, Yan Li, Xin Zhou, Shun Qiao, Dewu Han
Cell Biochemistry and Function.2019; 37(3): 161. CrossRef - Ropivacaine regulates the expression and function of heme oxygenase-1
Xiangbiao Yan, Yu Li, Xuechang Han, Xu Dong, Yajie Zhang, Qunzhi Xing
Biomedicine & Pharmacotherapy.2018; 103: 284. CrossRef - A review on heme oxygenase-1 induction: is it a necessary evil
Ajaz Ahmad Waza, Zeenat Hamid, Sajad Ali, Shabir Ahmad Bhat, Musadiq Ahmad Bhat
Inflammation Research.2018; 67(7): 579. CrossRef - Diabetes and Alzheimer's Disease: Mechanisms and Nutritional Aspects
Hee Jae Lee, Hye In Seo, Hee Yun Cha, Yun Jung Yang, Soo Hyun Kwon, Soo Jin Yang
Clinical Nutrition Research.2018; 7(4): 229. CrossRef - Social, economic, and policy implications of organ preservation advances
Alyssa Ward, David K. Klassen, Kate M. Franz, Sebastian Giwa, Jedediah K. Lewis
Current Opinion in Organ Transplantation.2018; 23(3): 336. CrossRef - Geniposide protects pancreatic β cells from high glucose‐mediated injury by activation of AMP‐activated protein kinase
Chunyan Liu, Yanan Hao, Fei Yin, Yonglan Zhang, Jianhui Liu
Cell Biology International.2017; 41(5): 544. CrossRef - Eff ects of hemin, a heme oxygenase-1 inducer in L-arginine-induced acute pancreatitis and associated lung injury in adult male albino rats
N. M. Aziz, M. Y. Kamel, R. A. Rifaai
Endocrine Regulations.2017; 51(1): 20. CrossRef - Downregulation of microRNA-155 ameliorates high glucose-induced endothelial injury by inhibiting NF-κB activation and promoting HO-1 and NO production
Xi Zhang, Xiangyang Liu, Yang Li, Jingbo Lai, Nana Zhang, Jie Ming, Xianjie Ma, Qiuhe Ji, Ying Xing
Biomedicine & Pharmacotherapy.2017; 88: 1227. CrossRef - Sulforaphane Protects against High Cholesterol-Induced Mitochondrial Bioenergetics Impairments, Inflammation, and Oxidative Stress and Preserves Pancreaticβ-Cells Function
Catalina Carrasco-Pozo, Kah Ni Tan, Martin Gotteland, Karin Borges
Oxidative Medicine and Cellular Longevity.2017; 2017: 1. CrossRef - Aromatic malononitriles stimulate the resistance of insulin-producing beta-cells to oxidants and inflammatory cytokines
Kyril Turpaev, Nils Welsh
European Journal of Pharmacology.2016; 784: 69. CrossRef - Differences in insulin biosynthesis pathway between small and large islets do not correspond to insulin secretion
Han-Hung Huang, Lisa Stehno-Bittel
Islets.2015; 7(5): e1129097. CrossRef - A newly identified polysaccharide from Ganoderma atrum attenuates hyperglycemia and hyperlipidemia
Kexue Zhu, Shaoping Nie, Chuan Li, Suli Lin, Mengmeng Xing, Wenjuan Li, Deming Gong, Mingyong Xie
International Journal of Biological Macromolecules.2013; 57: 142. CrossRef - Glycated Albumin Causes Pancreatic β-Cells Dysfunction Through Autophagy Dysfunction
Young Mi Song, Sun Ok Song, Young-Hye You, Kun-Ho Yoon, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee, Ji-Won Kim, Byung-Wan Lee
Endocrinology.2013; 154(8): 2626. CrossRef - Chronic Resveratrol Treatment Protects Pancreatic Islets against Oxidative Stress in db/db Mice
Young-Eun Lee, Ji-Won Kim, Eun-Mi Lee, Yu-Bae Ahn, Ki-Ho Song, Kun-Ho Yoon, Hyung-Wook Kim, Cheol-Whee Park, Guolian Li, Zhenqi Liu, Seung-Hyun Ko, Kathrin Maedler
PLoS ONE.2012; 7(11): e50412. CrossRef
- Diabetes: Risk factor and translational therapeutic implications for Alzheimer's disease
- Decreased Expression and Induced Nucleocytoplasmic Translocation of Pancreatic and Duodenal Homeobox 1 in INS-1 Cells Exposed to High Glucose and Palmitate
- Gyeong Ryul Ryu, Jun Mo Yoo, Esder Lee, Seung-Hyun Ko, Yu-Bae Ahn, Ki-Ho Song
- Diabetes Metab J. 2011;35(1):65-71. Published online February 28, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.1.65
- 3,033 View
- 37 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Type 2 diabetes mellitus (T2DM) is often accompanied by increased levels of circulating fatty acid. Elevations in fatty acids and glucose for prolonged periods of time have been suggested to cause progressive dysfunction or apoptosis of pancreatic beta cells in T2DM. However, the precise mechanism of this adverse effect is not well understood.
Methods INS-1 rat-derived insulin-secreting cells were exposed to 30 mM glucose and 0.25 mM palmitate for 48 hours.
Results The production of reactive oxygen species increased significantly. Pancreatic and duodenal homeobox 1 (Pdx1) expression was down-regulated, as assessed by reverse transcription-polymerase chain reaction and Western blot analyses. The promoter activities of insulin and Pdx1 were also diminished. Of note, there was nucleocytoplasmic translocation of Pdx1, which was partially prevented by treatment with an antioxidant, N-acetyl-L-cysteine.
Conclusion Our data suggest that prolonged exposure of beta cells to elevated levels of glucose and palmitate negatively affects Pdx1 expression via oxidative stress.
-
Citations
Citations to this article as recorded by- Nrf2 Activation Protects Mouse Beta Cells from Glucolipotoxicity by Restoring Mitochondrial Function and Physiological Redox Balance
Johanna Schultheis, Dirk Beckmann, Dennis Mulac, Lena Müller, Melanie Esselen, Martina Düfer
Oxidative Medicine and Cellular Longevity.2019; 2019: 1. CrossRef - Early overnutrition reduces Pdx1 expression and induces β cell failure in Swiss Webster mice
Maria M. Glavas, Queenie Hui, Eva Tudurí, Suheda Erener, Naomi L. Kasteel, James D. Johnson, Timothy J. Kieffer
Scientific Reports.2019;[Epub] CrossRef - Anti-diabetic effect of mulberry leaf polysaccharide by inhibiting pancreatic islet cell apoptosis and ameliorating insulin secretory capacity in diabetic rats
Yao Zhang, Chunjiu Ren, Guobing Lu, Zhimei Mu, Weizheng Cui, Huiju Gao, Yanwen Wang
International Immunopharmacology.2014; 22(1): 248. CrossRef - The Furan Fatty Acid Metabolite CMPF Is Elevated in Diabetes and Induces β Cell Dysfunction
Kacey J. Prentice, Lemieux Luu, Emma M. Allister, Ying Liu, Lucy S. Jun, Kyle W. Sloop, Alexandre B. Hardy, Li Wei, Weiping Jia, I. George Fantus, Douglas H. Sweet, Gary Sweeney, Ravi Retnakaran, Feihan F. Dai, Michael B. Wheeler
Cell Metabolism.2014; 19(4): 653. CrossRef
- Nrf2 Activation Protects Mouse Beta Cells from Glucolipotoxicity by Restoring Mitochondrial Function and Physiological Redox Balance
- Transdifferentiation of Enteroendocrine K-cells into Insulin-expressing Cells.
- Esder Lee, Jun Mo Yu, Min Kyung Lee, Gyeong Ryul Ryu, Seung Hyun Ko, Yu Bae Ahn, Sung Dae Moon, Ki Ho Song
- Korean Diabetes J. 2009;33(6):475-484. Published online December 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.6.475
- 2,224 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Despite a recent breakthough in human islet transplantation for treating type 1 diabetes mellitus, the limited availability of donor pancreases remains a major obstacle. Endocrine cells within the gut epithelium (enteroendocrine cells) and pancreatic beta cells share similar pathways of differentiation during embryonic development. In particular, K-cells that secrete glucose-dependent insulinotropic polypeptide (GIP) have been shown to express many of the key proteins found in beta cells. Therefore, we hypothesize that K-cells can be transdifferentiated into beta cells because both cells have remarkable similarities in their embryonic development and cellular phenotypes. METHODS: K-cells were purified from heterogeneous STC-1 cells originating from an endocrine tumor of a mouse intestine. In addition, a K-cell subclone expressing stable Nkx6.1, called "Kn4-cells," was successfully obtained. In vitro differentiation of K-cells or Kn4-cells into beta cells was completed after exendin-4 treatment and serum deprivation. The expressions of insulin mRNA and protein were examined by RT-PCR and immunocytochemistry. The interacellular insulin content was also measured. RESULTS: K-cells were found to express glucokinase and GIP as assessed by RT-PCR and Western blot analysis. RT-PCR showed that K-cells also expressed Pdx-1, NeuroD1/Beta2, and MafA, but not Nkx6.1. After exendin-4 treatment and serum deprivation, insulin mRNA and insulin or C-peptide were clearly detected in Kn4-cells. The intracellular insulin content was also increased significantly in these cells. CONCLUSION: K-cells are an attractive potential source of insulin-producing cells for treatment of type 1 diabetes mellitus. However, more experiments are necessary to optimize a strategy for converting K-cells into beta cells. -
Citations
Citations to this article as recorded by- Reprogramming of enteroendocrine K cells to pancreatic β-cells through the combined expression of Nkx6.1 and Neurogenin3, and reaggregation in suspension culture
Esder Lee, Gyeong Ryul Ryu, Sung-Dae Moon, Seung-Hyun Ko, Yu-Bae Ahn, Ki-Ho Song
Biochemical and Biophysical Research Communications.2014; 443(3): 1021. CrossRef
- Reprogramming of enteroendocrine K cells to pancreatic β-cells through the combined expression of Nkx6.1 and Neurogenin3, and reaggregation in suspension culture
- Differentiation of Pancreatic beta Cells from Human Pancreatic Duct Cells Derived from a Partial Pancreas Tissue.
- Ki Ho Song, Myung Mee Kim, Min Kyung Lee, Gyeong Ryul Ryu, Seung Hyun Ko, Sung Dae Moon, Yu Bae Ahn, Kun Ho Yoon, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang, Hyung Min Chin
- Korean Diabetes J. 2007;31(3):236-242. Published online May 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.3.236
- 1,961 View
- 23 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Despite a recent breakthrough in human islet transplantation for treating diabetes mellitus, the limited availability of insulin-producing tissue is still a major obstacle. This has led to a search for alternative sources of transplantable insulin-producing cells including pancreatic duct cells. We aimed to establish in vitro culture of pancreatic duct cells from a partial pancreas tissue in human, which could be harnessed to differentiate into pancreatic beta cells. METHODS: We isolated pancreatic duct cells from small pieces of pancreas tissue (1~3 g) derived from non-diabetic humans (n = 8) undergoing pancreatic surgery due to cancer. Pancreas tissue was finely minced after injection of collagenase P into the parenchyma. The mince was incubated in a shaking water bath at 37degrees C for 25 min and passed through a 150 micrometer mesh. The released cells were recovered, washed, and plated in a dish containing CMRL culture medium with serum. RESULTS: Isolated pancreatic cells grew in monolayer and became confluent in 1~2 wks showing typical epithelial cobblestone morphology. Immunochemistry demonstrated that ~90% of the cultured cells were cytokeratin7-positive duct cells. To induce beta cell differentiation, the cells were incubated in DMEM/F12 culture medium without serum. In addition, treatment with Matrigel overlay, exendin-4, cholera toxin or forskolin was done. Though beta cell differentiation was found by immunostaining and RT-PCR, the differentiation efficiency was very low. Over-expression of neurogenin-3 by recombinant adenovirus did not increase beta cell differentiation of the cultured duct cells significantly. CONCLUSION: We established in vitro culture of pancreatic duct cells from a partial pancreas tissue in human, which differentiate into pancreatic cells. However, a strategy to optimize beta cell differentiation in this model is needed. -
Citations
Citations to this article as recorded by- Transdifferentiation of Enteroendocrine K-cells into Insulin-expressing Cells
Esder Lee, Jun Mo Yu, Min Kyung Lee, Gyeong Ryul Ryu, Seung-Hyun Ko, Yu-Bae Ahn, Sung-Dae Moon, Ki-Ho Song
Korean Diabetes Journal.2009; 33(6): 475. CrossRef
- Transdifferentiation of Enteroendocrine K-cells into Insulin-expressing Cells
- The Role of cAMP/PKA Activation on Exendin-4-Induced Cyclin D1 Expression in INS-1 Cell.
- Gyeong Ryul Ryu, Jung Hoon Kang, Hwa In Jang, Seung Hyun Ko, In Kyung Jeong, Duck Joo Rhie, Shin Hee Yoon, Sang June Hahn, Yang Hyeok Jo, Myung Suk Kim, Myung Jun Kim
- Korean Diabetes J. 2005;29(4):295-303. Published online July 1, 2005
- 1,238 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Glucagon-like peptide-1(GLP-1) and exendin-4(EX-4) have been known to induce pancreatic islet proliferation and increases in the betacell mass. Cyclin D1 is a key protein responsible for the entry of the G into the S phase, thereby contributing to cell proliferation. Therefore, the effect of EX-4 on the expression of cyclin D1 in INS-1 cells, a rat pancreatic betacell line, was investigated. The involvement of either mitogen-activated protein kinases(MAPKs) or cyclic adenosine 5'-monophosphate/protein kinase A(cAMP/ PKA) in the EX-4-induced cyclin D1 expression was also examined. METHODS: INS-1 cells were treated with EX-4 (10 nM), and the cyclin D1 protein levels then determined by Western blot. To investigate the involvement of MAPKs in the EX-4- induced cyclin D1 expression, either a combined treatment of MAPKs inhibitors or transient transfection of extracellular signal-regulated kinase-1 (ERK1) was performed. The effect of cAMP on the EX-4-induced cyclin D1 expression was also examined by treatments with forskolin, an adenylyl cyclase activator, and H-89, a PKA inhibitor. RESULTS: EX-4 increased the expression of cyclin D1 protein in a dose-dependent manner. Although EX-4 induced phosphorylation of ERK1/2, the treatment with PD 98059 or the overexpression of ERK1 had no effect on the EX-4-induced cyclin D1 expression. However, forskolin significantly induced the expression of cyclin D1, whereas the pretreatment of H-89 inhibited the EX-4-induced cyclin D1 expression. CONCLUSION: These results suggest that EX-4 induce cyclin D1 expression in INS-1 cells via cAMP/PKA pathway, but this is not due to ERK activation.
- The Inhibitory Effect of Epicatechin on IL-1beta -induced iNOS Expression and NO Production in RINm5F Cell.
- Gyeong Ryul Ryu, Do Sik Min, Duck Joo Rhie, Shin Hee Yoon, Sang June Hahn, Myung Suk Kim, Yang Hyeok Jo, Myung Jun Kim
- Korean Diabetes J. 2003;27(6):456-466. Published online December 1, 2003
- 969 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Interleukin-1beta (IL-1beta ) stimulates the expression of inducible nitric oxide synthase (iNOS) and the production of nitric oxide (NO), lead to NO-mediated insulin, which produces cell damage. Within these signal pathways, nuclear factor-kappaB (NF-kappaB) activation is crucial, with many IL-1beta -sensitive genes containing NF-kappaB binding sites in their promoter regions. The inhibitory effect of (-)epicatechin (EC), an antioxidant agent, on IL-1beta -induced NF-kappaB activation, and the subsequent iNOS expression in RINm5F cells, were examined. METHODS: RINm5F cells were pretreated with EC (0.8 mM), and then cultured with IL-1beta (10U/mL), and the iNOS mRNA and protein levels then determined by Northern and Western blots, respectively. The production of NO was measured as nitrite in the culture supernatant. The protein levels of the inhibitor of nuclear factor kappaB (IkappaB) and NF-kappaB DNA binding activity were determined by Western blot and electrophoretic mobility shift assay, respectively. Also, the promoter activity following transient transfection of the iNOS promoter-luciferase reporter genes into the cells were tested. RESULTS: EC was found to significantly reduce the IL-1beta -induced NO production, and iNOS protein and mRNA levels, and also blocked the IL-1beta -induced IkappaB protein degradation, NF-kappaB activation and iNOS promoter activity. CONCLUSION: These results suggest that EC inhibits the IL-1beta -induced iNOS expression in RINm5F cells, by interfering with the binding of the NF-kappaB to the iNOS promoter, thereby inhibiting the induction of iNOS transcription.

 KDA
KDA
 First
First Prev
Prev





